Hospitals are improving patient care and cutting emergency room (ER) visits by implementing AI+EQ, a model that blends artificial intelligence with human empathy. This strategic approach pairs machine learning with emotional intelligence, allowing healthcare providers to automate administrative tasks and dedicate more time to direct patient interaction. Clinicians refer to this strategy as ‘AI+EQ,’ a framework designed to keep complex algorithms operating in the background, ensuring that human caregivers remain the primary focus of the patient experience.
Early wins from AI+EQ programs
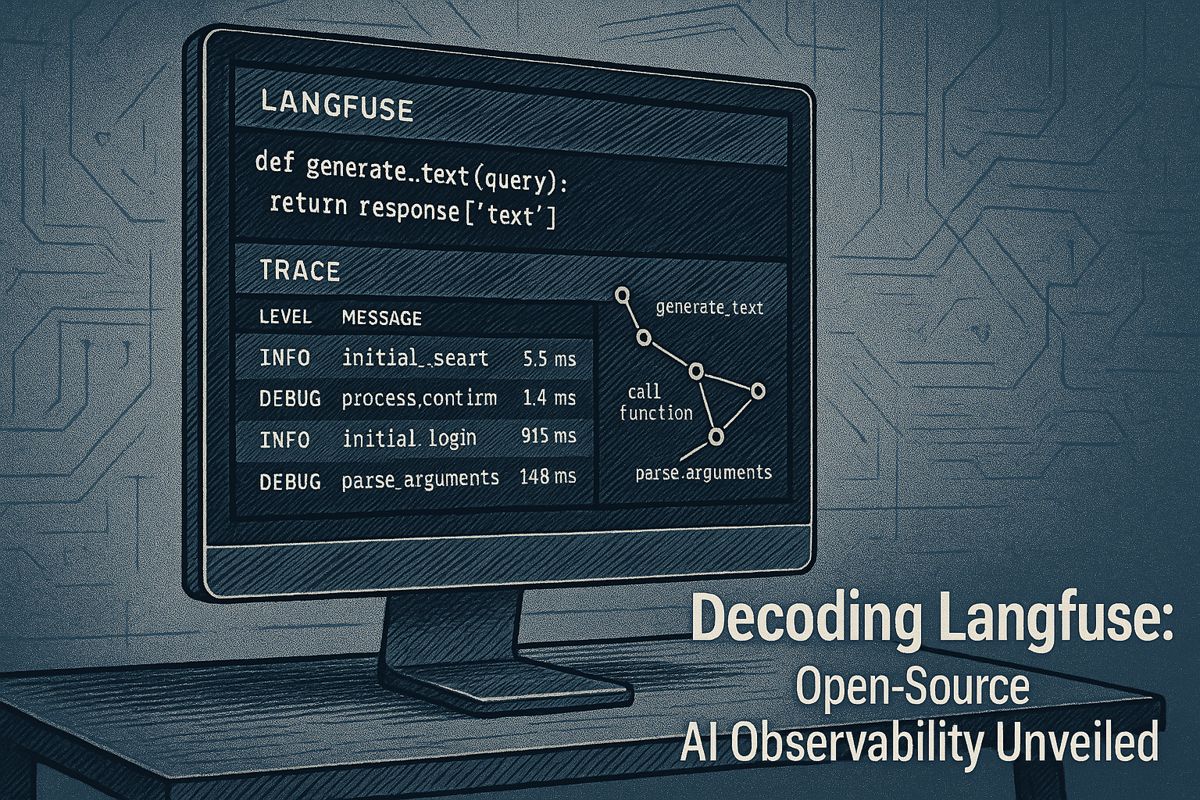
AI+EQ is a healthcare model where artificial intelligence handles repetitive, data-heavy tasks like paperwork and chart analysis. This frees up clinicians to focus on human-centric duties, such as patient counseling and empathetic communication, thereby improving the quality and efficiency of care without increasing staff workload.
For instance, physicians at the Mayo Clinic use an IBM Watson engine to analyze genomics and patient histories, leading to faster oncology treatment decisions and more time for patient counseling, as detailed in a Mayo Clinic case study. Similarly, University of Missouri Health Care utilizes Cerner’s embedded AI to auto-complete billing codes, reducing documentation hours and identifying potential safety gaps before prescriptions are filled.
The most significant results are seen in home care. An NCBI 2025 Watch List report found that providers using the AlayaCare remote monitoring platform achieved a 68% reduction in ER visits and a 35% decrease in hospitalizations for chronic disease patients. Instant alerts enable nursing teams to respond within minutes, offering immediate support.
Why AI+EQ matters in 2025
The importance of this model is growing. While global surveys show 80% of health executives consider AI critical, patient trust remains rooted in compassionate care. Highlighting this synergy, Emirates Health Services CIO Mubaraka Ibrahim reported at the 2025 World Health Expo that ambient AI reduced documentation time by 41% and increased direct patient interaction by 22%, proving that technology can scale empathy.
Design principles that keep empathy alive
- Prioritize Automation for Simple Tasks: Begin with single-click functions like scheduling and prior authorizations.
- Ensure Human Interpretation: Route all AI-generated insights to clinicians who can explain them to patients in understandable terms.
- Measure Empathy: Track success using metrics such as conversation duration and shared decision-making scores.
- Invest in Dual Training: Equip staff with skills in both data literacy and empathetic communication.
- Provide Clear Opt-Outs: Allow patients to easily opt out of any algorithmic recommendation.
The workforce angle
Addressing clinician burnout is a key aspect of AI+EQ. While rapid implementation can lead to ‘AI exhaustion,’ a thoughtful rollout offers significant benefits. For example, ambient documentation tools can save clinicians up to two hours per day. Institutions that integrate these automation initiatives with staff wellness programs observe improved retention rates and reduced absenteeism.
How providers can start
- Analyze the Patient Journey: Identify specific points in the care process where staff experience time pressure.
- Implement Low-Risk Automation First: Start with simple processes, like digitizing faxes, before moving to complex clinical decision support.
- Establish an Empathy Council: Form a multidisciplinary team to review patient-facing technologies, such as chatbot scripts and digital interfaces.
- Track and Report Progress: Publish annual dashboards showing both efficiency improvements and metrics related to human connection and patient satisfaction.
Ultimately, emerging data indicates that AI+EQ is more a governance philosophy than a specific technology stack. Healthcare systems that successfully balance computational power with human compassion are demonstrating superior results in patient outcomes, loyalty, and clinician morale.
What exactly is “AI+EQ” in hospital care?
It’s the deliberate pairing of AI-driven efficiency with human emotional intelligence. Algorithms handle repetitive data work – triage scoring, chart reviews, medication alerts – while clinicians use the freed minutes to sit eye-level with patients, ask open questions and respond to fears. Early pilots show the combo restores up to 22 % more face-to-face time without adding staff.
Where has this approach cut ER visits by 68 %?
Home-care networks using the AlayaCare platform report that figure after three months of remote monitoring for COPD and heart-failure patients. Machine-learning models flag early deterioration, outreach nurses call within minutes, and emergency transport drops sharply. Hospitalizations fell 35 % in the same cohort.
How do hospitals keep clinician empathy when bots are reading X-rays?
Three design rules are spreading:
1. Humans stay the messenger – AI may suggest, but a doctor or nurse still explains results.
2. “Empathy minutes” are scheduled – documentation time saved is blocked for conversation, not reassigned to new tasks.
3. Feedback loops – patient trust scores are collected weekly and fed back to the development team to refine tone and timing of AI alerts.
Does automation raise or lower staff burnout?
The answer is both. Facilities that added ambient documentation AI saw documentation burden fall 41 % and overtime claims drop. Yet units that rolled out multiple new tools every quarter recorded 45 % burnout among heavy AI users versus 35 % among infrequent users. Success hinges on paced roll-outs, shadow shifts and optional opt-in, not mandatory adoption.
What governance steps protect patient trust?
Leaders are adopting “explain-before-predict” protocols: patients hear what data the model uses and can request human review. Audit trails are open to accreditation teams, and equity dashboards track whether AI recommendations vary by race, gender or ZIP code. Early adopters publish quarterly safety bulletins to keep the social contract transparent.